Ozempic Side Effects Cause Disfigurement And £100m NHS Bill
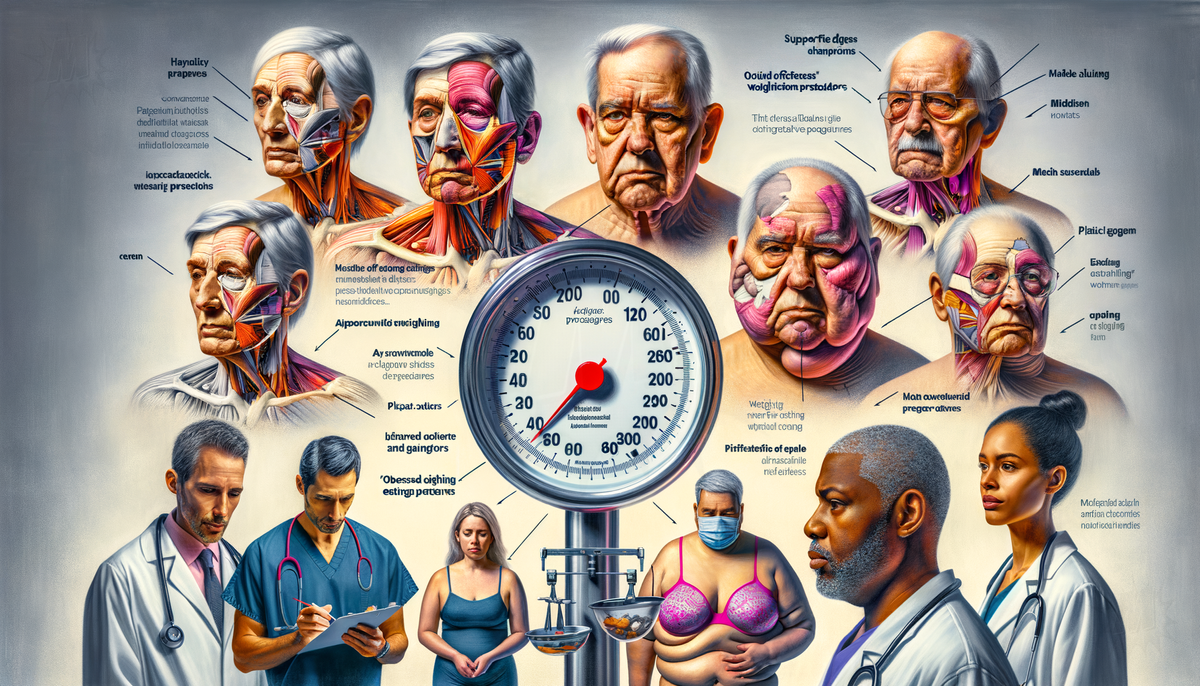
The NHS is confronting substantial financial implications as a result of the weight loss drug Ozempic, with estimates suggesting that tackling associated health complications could cost over £100 million annually. Ozempic, which is also used as a treatment for Type 2 diabetes, has been linked to significant side effects following rapid weight loss. These side effects include skin that appears 'melted' due to sagging, 'empty' breasts often referred to as 'Ozempic breasts,' gaunt facial features, and hair loss. While these issues are primarily cosmetic, they can profoundly affect an individual's health, especially in middle-aged and older users.
Plastic surgeons have observed an increase in patients seeking reconstructive procedures following weight loss induced by Ozempic. Previously, such surgeries were commonly associated with post-major weight loss surgeries like gastric bypass. The British Association of Plastic, Reconstructive and Aesthetic Surgeons (BAPRAS) has called on health authorities to broaden the availability of surgeries that remove excess skin.
The use of Ozempic has raised concerns among experts about the drug's potential negative impact on those with eating disorders. The possibility of weight regain after discontinuation could lead to disordered eating patterns and rebound weight gain, affecting metabolism, cardiovascular health, and self-image. Despite the issues, some research suggests that Ozempic might aid individuals with binge eating disorder (BED) by curbing cravings and appetite.
For patients experiencing 'deflated' breasts due to rapid fat loss, options such as supportive bras or plastic surgery may be considered. A study has found that after stopping GLP-1 agonist drugs like Ozempic, participants regained two-thirds of the weight they had lost within the first year, highlighting the potential for a cycle of weight loss and gain.