Medicare Advantage Profits Surge Amid Coverage Decisions for 2025
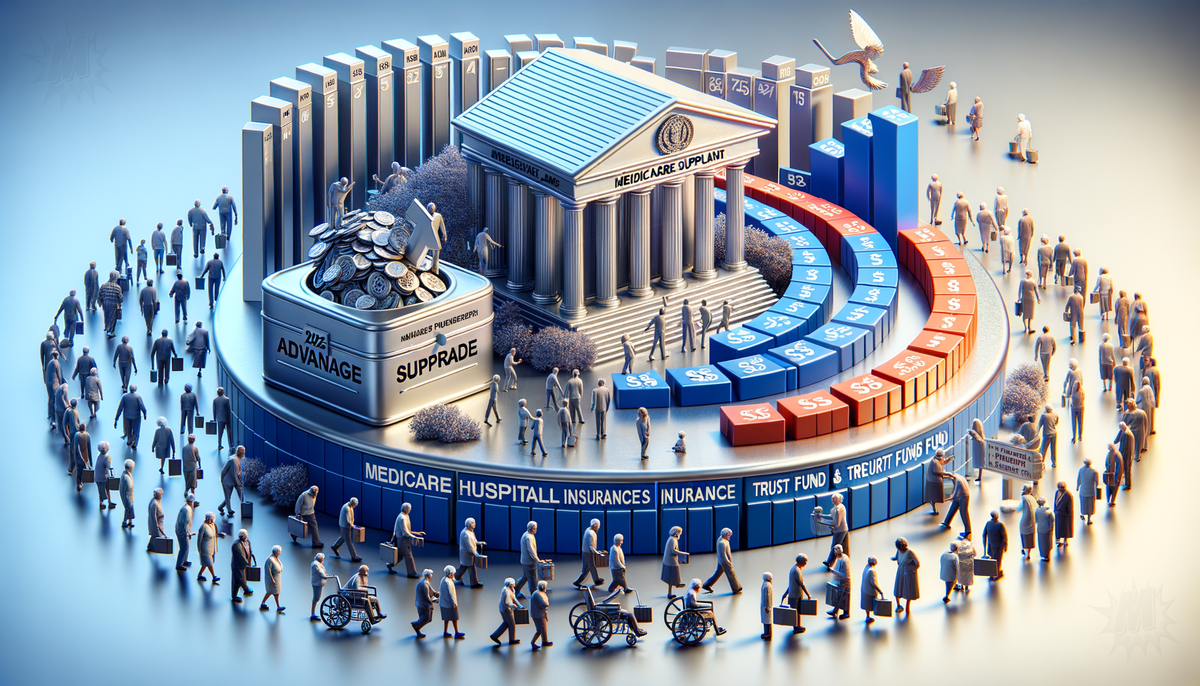
Industry experts are forecasting significant rate increases for Medicare Supplement plans in 2025, with most plans expected to rise by 9 percent or more. The increase is attributed to inflation and the migration of healthy individuals to Medicare Advantage plans, which places price pressure on those remaining in Medicare Supplement plans. Although the Annual Election Period (AEP) for these changes ends in December, companies typically announce their rate increases post-AEP. Healthy individuals who switch to another Medicare Supplement insurance company outside of AEP may save money, but the overall impact of the Inflation Reduction Act, medical inflation, and the shift to Medicare Advantage will lead to higher prices across all Medicare Supplement companies.
In 2023, the U.S. spent $1.04 trillion on Medicare, averaging over $3,000 per citizen, according to the Congressional Budget Office. Since its inception in 1965, the program has grown significantly and is projected to exceed $1.6 trillion by 2032. The Medicare Hospital Insurance Trust Fund, a major financing source for Medicare, is expected to be depleted by 2028, potentially leaving millions without adequate coverage. Contributing factors to these costs include government inefficiency and a fee-for-service model that encourages unnecessary procedures. The American Medical Association estimates that 25% of Medicare spending, about $250 billion annually, is wasted on overtreatment and administrative inefficiencies. The aging population is also adding strain to the system, prompting suggestions for a market-based approach to drive innovation and improve care quality.
The Medicare Advantage market reported the highest gross margins in the health insurance industry in 2023, according to the non-profit healthcare policy organization KFF. Private payers serving the federally funded program generated a gross margin of $1,982 per member, compared to $753 per enrollee for Medicaid. Major operators in the Medicaid market include Centene (CNC), Elevance Health (ELV), and Molina Healthcare (MOH). Despite a recent increase in demand for medical care among Medicare enrollees, the gross margin in the Medicare Advantage market remained largely consistent with 2022 levels. The report also emphasized the medical loss ratio, which measures the share of premiums that health insurers pay for members' medical costs.
Federal employees are advised to understand the correct enrollment rules for Medicare Parts A and B upon retirement. While some suggest enrolling in both parts at retirement, others argue that Federal Employees Health Benefits (FEHB) provide sufficient coverage. Federal employees with FEHB coverage who continue working past age 65 do not need to enroll in Part B immediately,